As acupuncture becomes a widely accepted therapy in pain management, stress relief, and overall health, the demand for skilled practitioners is growing across the U.S. From veterans seeking holistic care to individuals managing chronic pain, the acupuncture field is expanding rapidly. However, this growth brings an essential challenge: credentialing with Medicare, Medicaid, and commercial insurers. The process is complex, time-consuming, and essential for ensuring proper reimbursement.
If you’ve ever felt overwhelmed by the intricacies of Medicare’s Form 855B or endured lengthy delays in insurance approval, you’re not alone. Many acupuncturists face the same frustrations when navigating the credentialing maze. Understanding the importance of credentialing and the steps involved will help you avoid these pitfalls and ensure your practice receives timely reimbursements.
Why Credentialing Matters for Acupuncturists
Credentialing is the backbone of compliant, high-performing healthcare practices. Every practitioner, from primary care physicians to therapists and nurse practitioners, must have their licensure, certifications, and professional qualifications verified before joining a network.
Without proper credentialing:
-
Claims can be denied, delayed, or underpaid.
-
Practices risk regulatory scrutiny and audit penalties.
-
Patient trust and continuity of care can be disrupted.
Practices outsourcing credentialing and billing report 30–50% faster reimbursements and significantly fewer claim denials.
Credentialing and Re-credentialing
Credentialing verifies that a provider meets professional requirements for network participation, including:
-
Education and training
-
Licensure and board certifications
-
Work history and professional references
Re-credentialing occurs every 3 years to ensure credentials remain accurate and compliant with NCQA and payer standards.
Key Steps in Credentialing:
-
Submission of the CAQH Provider Data Portal application
-
Verification of licensure, malpractice insurance, and board certifications
-
Review by the Credentialing/Recredentialing Committee (CRC)
-
Approval or denial notification
How CAQH Simplifies Credentialing
The Council for Affordable Quality Healthcare (CAQH) provides a central portal for providers to input and update credentials. Health plans can access verified information in real-time, reducing the need for repetitive submissions.
Benefits of CAQH integration through CodeCure:
-
Eliminates repetitive submissions for each health plan.
-
Ensures updates are shared across networks in real-time.
-
Reduces errors that cause claim denials.
Acupuncture Market Insights
Data highlights the importance of credentialing for acupuncture practices:
-
The U.S. acupuncture market is projected to grow at a 14.2% CAGR from 2023 to 2030.
-
Over 90% of patients prefer practices that accept insurance and are properly credentialed.
-
Practices outsourcing credentialing report 30–50% faster reimbursements and fewer denials.
-
States like California, New York, Washington, Massachusetts, and Arizona have higher Medicaid coverage for acupuncture.
Understanding these numbers highlights the financial and operational impact of proper credentialing.
The Credentialing Process for Acupuncturists: Step-by-Step
Navigating the credentialing process can feel daunting, but breaking it down into clear steps helps simplify the journey. Here’s an overview of what you need to do:
Step 1: Gather Required Documentation
- Education and training certificates (e.g., NCCAOM)
- State licensure
- Malpractice insurance
- Professional references
- CPR/BLS certification (if required by payer)
Step 2: Submit Applications to Payers
- Medicare (Form 855B via PECOS)
- Medicare Advantage plans (Humana, Aetna, UnitedHealthcare)
- Medicaid (state-specific portals)
- Commercial insurers
Step 3: Verification
- Payors verify education, licensure, and work history through primary source verification.
Step 4: Committee Review & Contracting
- A credentialing committee reviews qualifications and issues a contract detailing reimbursement rates and billing guidelines.
Step 5: Recredentialing & Ongoing Maintenance
- Credentialing must be updated every 1-5 years, depending on the payer, to ensure continued network participation.
Pro Tip: Keeping a credentialing checklist ensures smoother approvals, fewer denials, and faster reimbursements.
Acupuncturist Credentialing Checklist
To streamline your credentialing, make sure you have these critical steps completed:
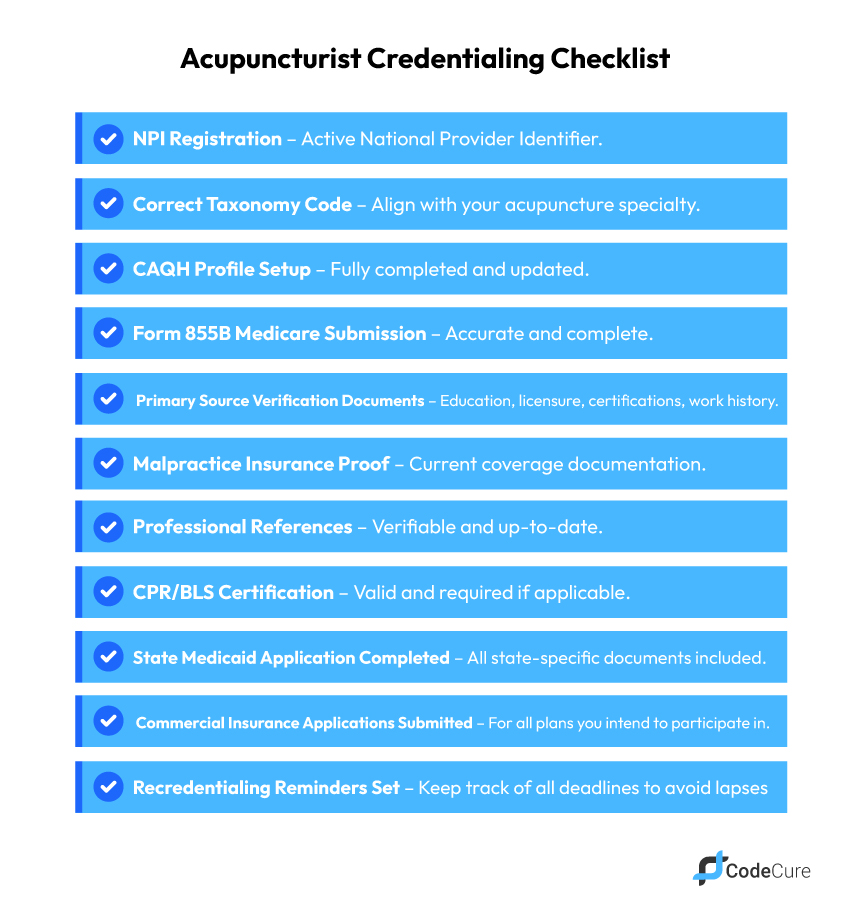
Keeping this checklist up-to-date ensures smoother approvals, fewer denials, and faster reimbursements.
Maintaining Compliance with Medicare, Medicaid, and State Regulations
Practices must monitor multiple compliance lists to avoid penalties:
-
Medicare Preclusion List – providers revoked or barred from Medicare.
-
NPDB & HIPDB – reportable actions for professional misconduct.
-
State Medicaid exclusions – NYSDOH or other state databases.
CodeCure automates compliance checks, alerts staff of updates, and prevents claims from being submitted to excluded providers.
Credentialing for Specialty Providers
Different provider types require unique documentation:
-
Behavioral Health: CAQH and Carelon Behavioral Health rules.
-
Midwives: Collaborative agreement with OB/GYN.
-
Lactation Consultants: NY Medicaid-approved certifications.
-
Nurse Practitioners & Physician Assistants: Licensure, certification, collaborative agreements (if required).
CodeCure tracks these requirements and automatically notifies the practice of missing documents.
Purpose: Captures niche audiences searching for specialty credentialing and builds authority.
Organizational Credentialing
Facilities like hospitals, dialysis centers, and outpatient rehab centers must meet additional requirements:
-
Current licensing and accreditation
-
Medicare/Medicaid certification
-
Malpractice coverage
-
Acceptable audit and inspection history
CodeCure consolidates all organizational and individual provider credentials, reducing administrative burden and ensuring compliance across multi-site practices.
Termination and Appeals Process
Providers may face termination for:
-
Loss or suspension of license or DEA number
-
Fraud or misrepresentation
-
Imminent patient harm
CodeCure tracks credentialing timelines, reports, and appeal deadlines, ensuring practices have proper documentation to defend or rectify credentialing issues.
Medicaid Credentialing: State-by-State Complexity
Medicaid rules differ across states, making credentialing a challenge for multi-state practices.
| State | Coverage Notes | Credentialing Notes |
| California | Chronic pain, PT adjunct | State Medicaid ID + CAQH profile required |
| New York | Chronic pain & mental health programs | PECOS or state portal submission |
| Washington | Chronic pain management | CAQH + state Medicaid portal |
| Massachusetts | Pain clinics only | Recredential every 3 years |
| Arizona | Chronic pain & integrative clinics | Maintain active NCCAOM certification |
Accurate state-by-state credentialing ensures timely claims and protects revenue.
Commercial Insurance Credentialing
Commercial payers add more complexity:
- Taxonomy code errors
- Missing or outdated CAQH profiles
- Confusion between credentialing approval and contract activation
- Frequent recredentialing requirements
Multi-state commercial credentialing requires constant monitoring to avoid denied claims.
Common Challenges in Acupuncture Credentialing & Billing
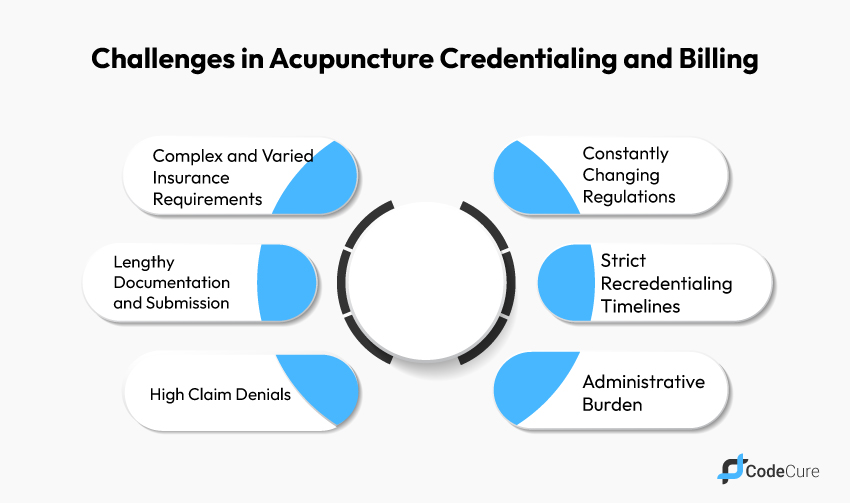
Managing credentialing and billing in an acupuncture practice is no small feat. Many providers face hurdles that can affect revenue, compliance, and even patient satisfaction. Understanding these challenges highlights why professional support is often necessary.
-
Complex and Varied Requirements: Each payer has unique rules and documentation standards.
-
Lengthy Documentation: Form 855B, CAQH, and state forms can take weeks to complete.
-
High Claim Denials: Errors in coding, taxonomy, or credentials disrupt cash flow.
-
Constantly Changing Regulations: CMS and state Medicaid rules frequently update.
-
Strict Recredentialing Timelines: Missing deadlines can suspend billing privileges.
-
Administrative Burden: Credentialing diverts staff from patient care.
Credentialing is not just a formality—it’s a strategic component of your practice’s financial health.
Outsourcing Credentialing and Billing: A Smart Solution
Managing credentialing and billing internally can be overwhelming. Outsourcing these tasks to experts can improve efficiency and reduce administrative burdens. Here’s why outsourcing is beneficial:
- Expertise and Accuracy: Credentialing professionals reduce errors in forms and documentation, ensuring faster approvals and reimbursements.
- Faster Approvals & Reimbursements: With streamlined submissions and proactive management, credentialing time is reduced, leading to quicker payments.
- Reduced Administrative Burden: Delegating these tasks allows your team to focus on patient care, improving both workflow and care quality.
- Seamless Integration with RCM: Outsourced credentialing integrates with your billing process to reduce claim denials and improve cash flow.
CodeCure: Streamlined Credentialing and Medical Billing Services
Managing credentialing and billing internally can be overwhelming. CodeCure offers comprehensive medical billing services and provider enrollment solutions tailored for acupuncturists and specialty providers.
Our Services Include:
-
Provider Enrollment: Credentialing and contracting with all commercial insurers and government payers
-
Medicare & Medicaid Enrollment & Revalidation
-
Credentials Verification: Physicians, acupuncturists, and ancillary healthcare providers
-
Network Management: For health plans and multi-site practices
-
Outsourced Hospital Privileging and medical staff office management
-
Managed Care Contracting
-
Annual Maintenance: CAQH updates, liability/licenses, and re-credentialing
-
Discounted Maintenance for Unlicensed Providers: QMHA, QMHP
-
Full Support for NPI & Group NPI Setup, Web Portal Setup
-
Coverage Across All States: Nationwide, including Alaska, Hawaii, and Puerto Rico.
Partnering with CodeCure ensures your practice runs efficiently while avoiding costly credentialing errors and claim delays.
Conclusion
Credentialing is essential for acupuncturists to secure timely reimbursements, expand patient access, and maintain regulatory compliance. By outsourcing to a trusted partner like CodeCure, you can streamline insurance enrollment, reduce administrative burden, and focus on providing excellent care.
Contact CodeCure today to begin your credentialing process and ensure your acupuncture practice operates smoothly and profitably.






