Get Credentialing Done Hassle-Free — and Free of Charge — This Holiday Season
Thanksgiving marks the start of holiday closures, staff shortages, and year-end administrative pressure for medical practices across the U.S. But what many practices don’t realize is this:
The weeks before Thanksgiving and Christmas are the most critical time of the year for payer credentialing and re-credentialing.
Payers like Medicare, Medicaid, Blue Cross, Aetna, and UnitedHealthcare slow down dramatically between late November and early January. That means applications submitted now may determine whether your practice goes into the new year fully enrolled or stuck waiting months for approvals, delayed reimbursements, and out-of-network claim rejections.
That’s why this Thanksgiving, CodeCURe is offering a limited-time Credentialing Support Special — hassle-free and free of charge.
So practices can head into 2026 fully credentialed, fully enrolled, and fully reimbursed.
Why Thanksgiving Is the Perfect Time to Handle Your Credentialing
Most practices think of credentialing as something to “get around to,” but the timing matters more than many realize.
Here’s why Thanksgiving season is the ideal window:
1. Payer Delays Spike After Mid-November
According to CMS and commercial payer data:
- Medicare applications submitted after November 20th face a 22–30% longer approval timeline.
- Commercial payers like Aetna and UHC experience 2–3x slower processing in December.
- Medicaid offices in states like Texas, Florida, New York, Georgia, and California slow down by nearly 40% due to holidays and state-level staffing shortages.
Submitting credentialing now means you avoid the January backlog, the worst time of year for enrollment delays.
2. Holiday Season = Minimal Staff Availability
PTO, holiday closures, limited internal credentialing staff all contribute to missed deadlines.
In many practices:
- Revalidations slip
- Address/location updates get missed
- CAQH isn’t refreshed
- Expiring licenses aren’t updated in payer portals
A credentialing gap during this season can easily turn into:
- Out-of-network claims
- Reimbursement holds
- Retroactive denials
- Delayed Medicare/Medicaid payments
3. Thanksgiving Is a Natural Administrative Checkpoint
Just as practices clean up their AR at year-end, Thanksgiving is a perfect moment to reset and ensure:
- Every provider is correctly enrolled
- All group contracts are active
- New providers are linked to tax IDs
- Expiring credentials are updated
- NPPES & CAQH are accurate and current
This makes December smoother and January profitable.
The Real Cost of Delayed or Incomplete Credentialing
Credentialing problems don’t just slow down admin work, they drain revenue.
Across the U.S., practices lose:
- $30,000–$70,000 per provider when credentialing is delayed
- $200,000+ in annual revenue for incomplete payer enrollment
- 15% of total collections due to out-of-network claims that should’ve been in-network
According to MGMA:
- 40% of claims for new providers are denied due to credentialing issues
- 68% of practices experience revenue loss from delayed CAQH updates
- 52% of providers start seeing patients before credentialing is complete
Meaning:
You’re delivering care, but you’re not being paid simply because a payer hasn’t approved your enrollment.
Specialties Impacted the Most During Credentialing Season
Credentialing delays hit certain specialties harder because of volume, payer mix, and complexity.
High-Risk Specialties Include:
- Primary Care (high patient volume)
- Behavioral Health (authorization & Medicaid heavy)
- Orthopedics (high-value claims)
- Cardiology (Medicare-driven reimbursements)
- Pain Management (strict documentation rules)
- Ophthalmology (payer-specific credentialing nuances)
- EMS/Ambulance (complex enrollment and state-specific rules)
- Dental & Oral Surgery (payer restrictions and slow Medicaid processing)
- Urgent Care (multiple providers, multiple payers, rotating staffing)
If your practice is in one of these specialties, November is your last window to avoid January-February reimbursement delays.
What Happens If You Don’t Fix Credentialing Before December?
Here are the real risks practices face when credentialing drags into the holiday season:
- Claims go out-of-network
- Payers delay linking providers to group contracts
- CAQH lapses cause automatic denials
- Medicare PECOS holds payments
- Medicaid state-specific rules stall applications
- Retroactive effective dates become harder to secure
- New providers cannot bill for weeks or months
- Providers cannot enroll with critical plans (BCBS, UHC, Aetna, Cigna, Humana)
A simple credentialing mistake today becomes a revenue emergency next year.
Thanksgiving Offer: Free Credentialing Support from CodeCURe
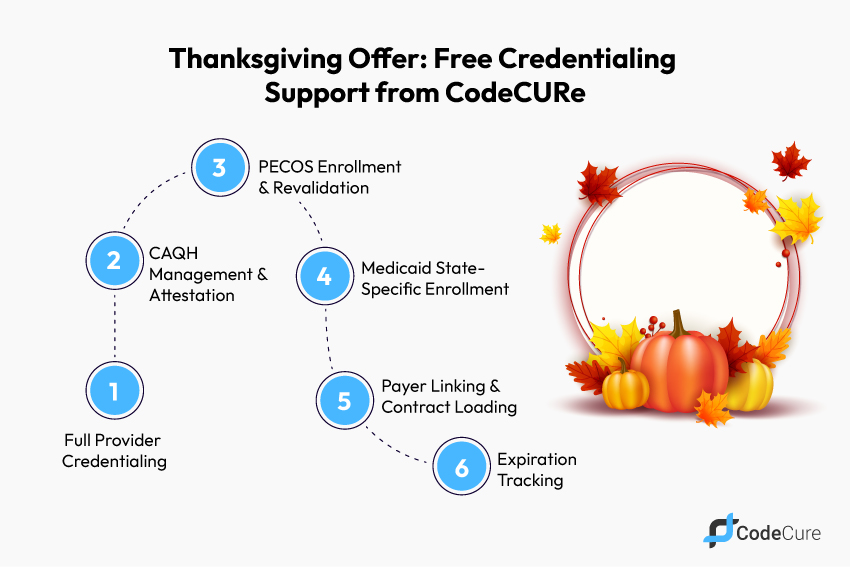
To support practices during the busiest credentialing season, CodeCURe is offering complimentary credentialing support for a limited time.
This includes:
✔ Full Provider Credentialing
For new or existing providers across Medicare, Medicaid, BCBS, UHC, Aetna, Cigna, Humana, and state-specific payers.
✔ CAQH Management & Attestation
We update, correct, and maintain your profile.
✔ PECOS Enrollment & Revalidation
For Medicare, including address updates and group reassignment.
✔ Medicaid State-Specific Enrollment
Texas, Florida, California, Georgia, New York, and more.
✔ Payer Linking & Contract Loading
Ensuring each provider is attached to each practice TIN.
✔ Expiration Tracking
Licenses, DEA, malpractice, CME, CAQH, and payer deadlines.
And yes — all of this credentialing support is FREE during the Thanksgiving Special.
What’s Buried in Your Credentialing Workload?
Before we take it off your plate, here’s what most practices are struggling with right now:
- Incomplete or incorrect CAQH profiles
- Missing documents required by commercial payers
- Providers working without being fully linked to group plans
- Medicaid revalidations near expiration
- Medicare PECOS enrollment errors
- Contract changes not reflected in payer systems
- Delayed EFT/ERA setup
- Provider location updates not processed
- Old data that triggers automatic denials
Credentialing mistakes don’t show up immediately; they appear months later as denials, payment holds, and underpayments.
Key Credentialing & Enrollment Statistics
| Credentialing & Enrollment Area | Statistic |
| Average payer processing time | 60–120 days |
| Medicare revalidation delays | Increase up to 30% in Nov–Dec |
| Commercial payer backlog | 2–3× higher in Q4 |
| CAQH-related denials | 24–40% of new provider claims |
| Medicaid denial rate | 21–29% depending on state |
| Lost revenue due to credentialing | $30k–$70k per provider |
These numbers highlight one truth:
Delaying credentialing during holiday season = guaranteed revenue loss.
How CodeCURe Helps
We don’t just “do credentialing.”
We remove the complexity and restore control to your practice.
Here’s how CodeCURe supports you at a high level:
✔ Credentialing Diagnostics
We identify missing elements, expirations, outdated details, and rejected applications.
✔ Payer-Specific Strategy
We navigate Medicare, Medicaid, BCBS, Aetna, UHC, Cigna, and Humana requirements without giving away our proprietary workflow.
✔ Process Streamlining
We show you where delays will occur and how to prevent them.
✔ Compliance Alignment
Ensuring you’re fully compliant with CMS and commercial payer rules.
✔ Ongoing Monitoring
We track deadlines, expirations, and revalidations so you never slip through the cracks again.
Thanksgiving Is the Season of Giving — Let CodeCURe Give You a Fresh Start
This holiday, you take care of your patients.
Let us take care of your credentialing.**
Practices that clean up their credentialing before December experience:
- Faster January reimbursements
- Better payer connectivity
- Fewer credentialing-related denials
- Higher clean-claim rates
- Smooth onboarding for new providers
- Stronger financial positioning for Q1
This is your chance to begin the new year:
✔ Fully credentialed
✔ Fully enrolled
✔ Fully paid
CTA: Claim Your Free Thanksgiving Credentialing Support
This holiday season, simplify your administrative burden and protect your revenue.
Claim your free Thanksgiving Credentialing Special with CodeCURe
and make sure every provider in your group starts the new year fully credentialed and financially ready.
Secure your spot; the offer is limited due to high demand.
FAQs:
Can you help if my provider is already seeing patients without being credentialed?
Yes, we help determine retroactive eligibility and correct payer linking.
How long does credentialing take during the holidays?
60–120 days, depending on the payer, which is why starting now is critical.
Does this include CAQH maintenance?
Yes, updates, attestation, document uploading, and corrections.
Will you manage PECOS revalidation?
Yes, Medicare PECOS setup, reassignments, revalidations, and updates are included.
What if my Medicaid enrollment has already expired?
We assist with reinstatement or re-enrollment, depending on state rules.
How do I get started?
Simply submit your provider list, NPI, TIN, and payer list, and we take it from there.






